The biceps muscle is attached to the bone at the elbow. The biceps muscle is inserted into the radial  tuberosity by the distal biceps tendon. The biceps muscle is responsible for some elbow flexion and is the primary supinator of the forearm. Supination is the function used when turning a key or a door knob. The biceps muscle is responsible for over 50% of forearm supination. Rupture of the distal biceps tendon involves flexion of the elbow against resistance with eccentric loading and sudden tearing of the tendon. The muscle may retract into the upper arm causing a bump or “Popeye” sign. If the ruptured tendon is not repaired, the patient will lose the ability to supinate the forearm adequately. Injury to the lateral antebrachial cutaneous nerve may occur when treating a distal biceps tendon rupture. The lateral antebrachial cutaneous nerve lies between the brachialis and biceps muscles. The nerve can become injured from aggressive retraction. The lateral antebrachial cutaneous nerve originates cutaneous nerve originates from the musculocutaneous nerve. Injury to the nerve results in loss of sensation along the radial aspect of the forearm.
tuberosity by the distal biceps tendon. The biceps muscle is responsible for some elbow flexion and is the primary supinator of the forearm. Supination is the function used when turning a key or a door knob. The biceps muscle is responsible for over 50% of forearm supination. Rupture of the distal biceps tendon involves flexion of the elbow against resistance with eccentric loading and sudden tearing of the tendon. The muscle may retract into the upper arm causing a bump or “Popeye” sign. If the ruptured tendon is not repaired, the patient will lose the ability to supinate the forearm adequately. Injury to the lateral antebrachial cutaneous nerve may occur when treating a distal biceps tendon rupture. The lateral antebrachial cutaneous nerve lies between the brachialis and biceps muscles. The nerve can become injured from aggressive retraction. The lateral antebrachial cutaneous nerve originates cutaneous nerve originates from the musculocutaneous nerve. Injury to the nerve results in loss of sensation along the radial aspect of the forearm.
Treatment of a distal biceps tendon injury usually requires surgery due to the important supination function of the biceps muscle. Surgery may be done in the form of a single anterior incision or a two incision technique. Both of these techniques have their advantages and disadvantages. The anterior approach is easier with minimal risk of synostosis; however, there is a risk of injury to the posterior interosseous nerve. The two incision approach has less risk of injury to the posterior interosseous nerve, however there is a risk of synostosis. The lateral antebrachial nerve is the nerve most commonly injured during repair of a distal biceps tendon rupture regardless of the technique that is used. When treating the distal biceps tendon rupture, identify and protect the lateral antebrachial cutaneous nerve. Diffuse pain and paresthesia in the forearm after distal biceps tendon repair should be investigated for lateral antebrachial cutaneous nerve injury. In this situation, the nerve may need to be explored.

 Avascular necrosis (AVN), or osteonecrosis, is death of a segment of bone due to disruption of the blood supply. Extraosseous or intraosseous interruption of the venous or arterial blood flow. AVN may be caused due to fractures of the femoral neck or dislocations of the hip, or due to mechanical disruption of blood vessels. Trauma to the deep branch of the Medial Femoral Circumflex Artery may occur with antegrade rod placement during piriformis entry in children. Posterior dislocation of the femoral head should be reduced in an expedited way to decrease the risk of thrombosis of the vessels which supply the femoral head. Osteonecrosis develops in about 2-20% of hips that are reduced within 6 hours. The risk of osteonecrosis will increase with delay in reduction of the hip. Osteonecrosis appears within two years after the injury. It is evident within one year in most patients.
Avascular necrosis (AVN), or osteonecrosis, is death of a segment of bone due to disruption of the blood supply. Extraosseous or intraosseous interruption of the venous or arterial blood flow. AVN may be caused due to fractures of the femoral neck or dislocations of the hip, or due to mechanical disruption of blood vessels. Trauma to the deep branch of the Medial Femoral Circumflex Artery may occur with antegrade rod placement during piriformis entry in children. Posterior dislocation of the femoral head should be reduced in an expedited way to decrease the risk of thrombosis of the vessels which supply the femoral head. Osteonecrosis develops in about 2-20% of hips that are reduced within 6 hours. The risk of osteonecrosis will increase with delay in reduction of the hip. Osteonecrosis appears within two years after the injury. It is evident within one year in most patients. 



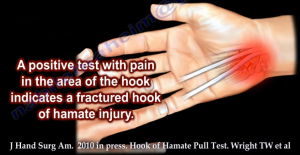
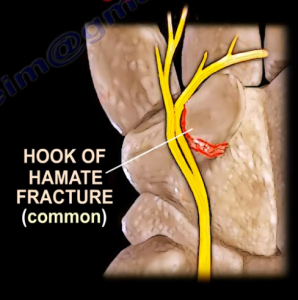 bones. The ulnar nerve can become injured by a fracture of the body (rare) or by a fracture of the hook (common) which may cause neuropathy of the ulnar nerve within the Guyon’s canal. Missing the fracture can lead to persistent pain from nonunion. Hamate hook fractures are most often seen in racquet, bat, or club sports such as hockey and golf. Fractures of the Hamate bone are difficult to diagnose and routine x-rays may not show the fracture. Hook fractures of the Hamate are best seen by carpal tunnel x-ray views; however, a CT scan is the best study. The physician should rule out the ossification center (os hamuli proprium).
bones. The ulnar nerve can become injured by a fracture of the body (rare) or by a fracture of the hook (common) which may cause neuropathy of the ulnar nerve within the Guyon’s canal. Missing the fracture can lead to persistent pain from nonunion. Hamate hook fractures are most often seen in racquet, bat, or club sports such as hockey and golf. Fractures of the Hamate bone are difficult to diagnose and routine x-rays may not show the fracture. Hook fractures of the Hamate are best seen by carpal tunnel x-ray views; however, a CT scan is the best study. The physician should rule out the ossification center (os hamuli proprium).