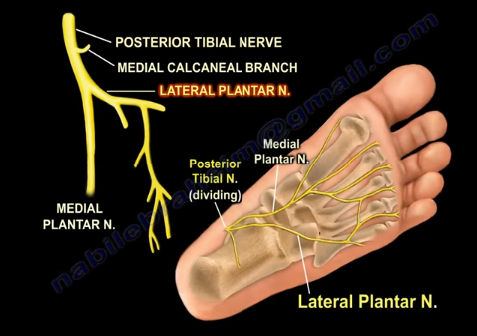
The lateral plantar nerve is branch of the posterior tibial nerve, which originates from the sciatic nerve. Around the medial side of the ankle, close to the tarsal tunnel, the posterior tibial nerve divides into the medial and lateral plantar nerves. 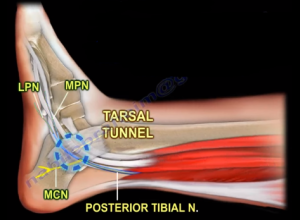
Thickening of the flexor retinaculum will cause compression of the posterior tibial nerve, which is called tarsal tunnel syndrome. When drawing a line between the medial malleolus and the calcaneus, the posterior tibial nerve divides into branches within 2 cm from this axis. The lateral plantar nerve is interesting because its branches give innervation to most of the intrinsic muscles in the foot—similar to the ulnar nerve in the hand. The lateral plantar nerve is also important due to its first branch being the Baxter’s nerve. 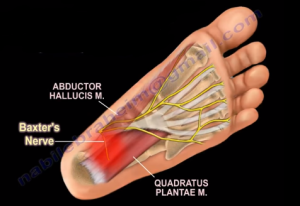
This nerve is always mentioned in nerve entrapment in running athletes and is associated with chronic heel related pain. The pain associated with the Baxter’s nerve is very similar to the pain associated with plantar fasciitis; the pain is in the same location, the mechanical symptoms are the same, and there is nerve pain unassociated with weight-bearing.
The first branch of the lateral plantar nerve gets compressed between the fascia of the abductor hallucis muscle and the medial side of the quadratus plantae muscle. This condition may require surgical release of the abductor hallucis fascia if conservative treatments and injections do not produce any effect.
In summary, the lateral plantar nerve:
- Is similar to the ulnar nerve in the hand
- Supplies most of the intrinsic muscles of the foot
- Supplies the Baxter’s nerve branch
- Can be injured during surgery (rod placement from the heel).
 Another point of interest when it comes to the lateral plantar nerve is the hardware placement. Hardware placement prominent to the sustentaculum tali can injure the flexor hallucis longus tendon and the lateral plantar nerve.
Another point of interest when it comes to the lateral plantar nerve is the hardware placement. Hardware placement prominent to the sustentaculum tali can injure the flexor hallucis longus tendon and the lateral plantar nerve.