Radial Nerve Anatomy
The radial nerve arises from the posterior cord of the brachial plexus and lies posterior to the axillary artery. The radial nerve receives branches from each nerve root from C5-T1. The radial nerve courses on the posterior wall of the axilla and lies on top of the subscapularis, the teres major, and the latissimus dorsi muscles. All three of these muscles (subscapularis-upper & lower subscapular n., teres major-lower subscapular n., latissimus dorsi-thoracodorsal n.) are supplied by the posterior cord of the brachial plexus. 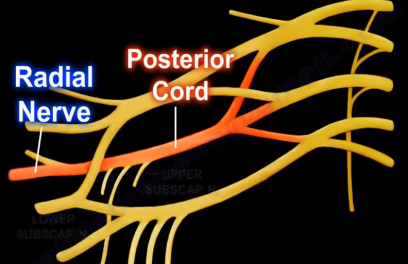 The radial nerve continues into the posterior compartment of the upper arm. The radial nerve then gives three branches in the axilla: branch to long head of triceps, branch to medial head of triceps, posterior cutaneous nerve of the arm. Some books show the position of the posterior cutaneous nerve of the arm may be higher than the branches to the triceps. The profunda brachii artery arises from the axillary artery. The radial nerve next travels through the triangular interval with the profunda brachii artery posteriorly. The radial nerve is bound proximally by the teres major, medially by the long head triceps, and laterally by the humeral shaft. It contains the profunda brachii artery and the radial nerve. The radial nerve enters the upper arm between the long head and the medial head of the triceps and then it runs towards the spiral groove of the humerus. The spiral groove is a thin, bare area of bone that lies in the upper 2/3 of the back of the humerus between the lateral and medial heads of the triceps. There are posterior safe zones of the humerus 10cm distal to the lateral acromion and 10cm proximal to the lateral epicondyle. Four branches arise from the radial nerve within the spiral groove.
The radial nerve continues into the posterior compartment of the upper arm. The radial nerve then gives three branches in the axilla: branch to long head of triceps, branch to medial head of triceps, posterior cutaneous nerve of the arm. Some books show the position of the posterior cutaneous nerve of the arm may be higher than the branches to the triceps. The profunda brachii artery arises from the axillary artery. The radial nerve next travels through the triangular interval with the profunda brachii artery posteriorly. The radial nerve is bound proximally by the teres major, medially by the long head triceps, and laterally by the humeral shaft. It contains the profunda brachii artery and the radial nerve. The radial nerve enters the upper arm between the long head and the medial head of the triceps and then it runs towards the spiral groove of the humerus. The spiral groove is a thin, bare area of bone that lies in the upper 2/3 of the back of the humerus between the lateral and medial heads of the triceps. There are posterior safe zones of the humerus 10cm distal to the lateral acromion and 10cm proximal to the lateral epicondyle. Four branches arise from the radial nerve within the spiral groove.  In the posterior approach, if the surgeon follows these cutaneous nerves proximally, it will lead to identification of the radial nerve itself. The radial nerve passes through the lateral intermuscular septum and enters the anterior compartment of the arm at least 7.5 cm above the elbow joint. Anteriorly, it runs between the brachialis and brachioradialis muscle anterior to the lateral epicondyle. This is the site for exposure of the radial nerve anteriorly (between the brachialis and brachioradialis muscles anteriorly). The radial nerve gives branches to supply the lateral part of the brachialis, brachioradialis, extensor carpi radialis longus, and the extensor carpi radialis brevis muscles. The radial nerve is vulnerable to injury below the spinal groove when there is a fracture in the distal third of the humeral shaft. Injury to the nerve will cause the condition of wrist drop. At about the level of the lateral epicondyle, the radial nerve begins to divide into the deep branch and the superficial branch of the radial nerve. The anconeus muscle is also innervated by the radial nerve. The posterior interosseous nerve (deep branch) enters the extensor compartment of the forearm between the two heads of the supinator muscle. The ulnar nerve enters the forearm by passing through the two heads of the flexor carpi ulnaris muscle and the median nerve enters the forearm by passing through the two heads of the pronator teres muscle.
In the posterior approach, if the surgeon follows these cutaneous nerves proximally, it will lead to identification of the radial nerve itself. The radial nerve passes through the lateral intermuscular septum and enters the anterior compartment of the arm at least 7.5 cm above the elbow joint. Anteriorly, it runs between the brachialis and brachioradialis muscle anterior to the lateral epicondyle. This is the site for exposure of the radial nerve anteriorly (between the brachialis and brachioradialis muscles anteriorly). The radial nerve gives branches to supply the lateral part of the brachialis, brachioradialis, extensor carpi radialis longus, and the extensor carpi radialis brevis muscles. The radial nerve is vulnerable to injury below the spinal groove when there is a fracture in the distal third of the humeral shaft. Injury to the nerve will cause the condition of wrist drop. At about the level of the lateral epicondyle, the radial nerve begins to divide into the deep branch and the superficial branch of the radial nerve. The anconeus muscle is also innervated by the radial nerve. The posterior interosseous nerve (deep branch) enters the extensor compartment of the forearm between the two heads of the supinator muscle. The ulnar nerve enters the forearm by passing through the two heads of the flexor carpi ulnaris muscle and the median nerve enters the forearm by passing through the two heads of the pronator teres muscle.  The area in which the posterior interosseous nerve passes through is called the “Arcade of Frohse” and this area is often a site of entrapment of the nerve. The posterior interosseous nerve supplies these muscles on the radial side and dorsal surface of the forearm: posterior interosseous n., posterior interosseous n. passes through the supinator m., extensor digiti minimi, extensor carpi ulnaris, extensor digitorum, extensor indicis, extensor pollicis brevis, extensor pollicis longus, and abductor pollicis longus. The posterior interosseous nerve does not supply cutaneous sensation and it is purely motor nerve. Injury to the posterior interosseous nerve will lead to inability of the patient to extend their fingers or “hitchhike” the thumb. During recovery from posterior interosseous nerve injury, the extensor digitorum muscle is the first one to recover and the extensor indicis is the last muscle to recover. The superficial radial nerve runs deep to the brachioradialis muscle. The superficial radial nerve continues until about 5cm above the wrist where it immerges from underneath the brachioradialis muscle, piercing the deep fascia and lying between the brachioradialis and the extensor carpi radialis longus muscles, then descending towards the anatomical snuff box. The superficial radial nerve is a sensory nerve supplying the majority of the dorsum of the hand. The sensory areas involving the cutaneous branches of the upper arm and forearm, and the superficial sensory radial nerve are shown here. Wartenberg’s Syndrome is characterized by entrapment of the superficial branch of the radial nerve above the wrist. The pain is located 8cm proximal to the radial styloid.
The area in which the posterior interosseous nerve passes through is called the “Arcade of Frohse” and this area is often a site of entrapment of the nerve. The posterior interosseous nerve supplies these muscles on the radial side and dorsal surface of the forearm: posterior interosseous n., posterior interosseous n. passes through the supinator m., extensor digiti minimi, extensor carpi ulnaris, extensor digitorum, extensor indicis, extensor pollicis brevis, extensor pollicis longus, and abductor pollicis longus. The posterior interosseous nerve does not supply cutaneous sensation and it is purely motor nerve. Injury to the posterior interosseous nerve will lead to inability of the patient to extend their fingers or “hitchhike” the thumb. During recovery from posterior interosseous nerve injury, the extensor digitorum muscle is the first one to recover and the extensor indicis is the last muscle to recover. The superficial radial nerve runs deep to the brachioradialis muscle. The superficial radial nerve continues until about 5cm above the wrist where it immerges from underneath the brachioradialis muscle, piercing the deep fascia and lying between the brachioradialis and the extensor carpi radialis longus muscles, then descending towards the anatomical snuff box. The superficial radial nerve is a sensory nerve supplying the majority of the dorsum of the hand. The sensory areas involving the cutaneous branches of the upper arm and forearm, and the superficial sensory radial nerve are shown here. Wartenberg’s Syndrome is characterized by entrapment of the superficial branch of the radial nerve above the wrist. The pain is located 8cm proximal to the radial styloid.
 The mortality rate in one year is about 25%. Surgery is usually needed to treat patients with femoral neck fractures. Very rarely the patient is treated without surgery and that can occur in patients with serious, significant medical issues. There is consensus that surgery should be done early and the outcome is better when the surgery is done within 48 hours of admission. Surgery is usually done once the medical condition of the patient is optimized. Sicker patients are usually admitted under the medical service. Younger, healthier patients are usually admitted under orthopedic care. Co-management is frequently done for these patients. Sometimes screening Doppler is done in delayed presentation to the hospital to diagnose DVT and to document its presence on admission that it occurred before the patient came to the hospital and that it is not a hospital acquired condition. While it is a clear cut or straight forward decision to save the femoral head in the younger patient and to do reduction (closed or open), this decision is variable in the elderly patient. This decision usually depends on the displacement of the fracture and the physiologic condition of the patient. The physiologic age of the patient determines the treatment and the risk of complication.
The mortality rate in one year is about 25%. Surgery is usually needed to treat patients with femoral neck fractures. Very rarely the patient is treated without surgery and that can occur in patients with serious, significant medical issues. There is consensus that surgery should be done early and the outcome is better when the surgery is done within 48 hours of admission. Surgery is usually done once the medical condition of the patient is optimized. Sicker patients are usually admitted under the medical service. Younger, healthier patients are usually admitted under orthopedic care. Co-management is frequently done for these patients. Sometimes screening Doppler is done in delayed presentation to the hospital to diagnose DVT and to document its presence on admission that it occurred before the patient came to the hospital and that it is not a hospital acquired condition. While it is a clear cut or straight forward decision to save the femoral head in the younger patient and to do reduction (closed or open), this decision is variable in the elderly patient. This decision usually depends on the displacement of the fracture and the physiologic condition of the patient. The physiologic age of the patient determines the treatment and the risk of complication.  The pre-injury cognitive and physiologic age and function determines the optimal function after hip fracture treatment. There is a consensus that if the fracture is nondisplaced, complete or incomplete fracture, then you will treat the fracture with screw fixation. Usually at least three screws are used. The surgery is a relatively small surgery. Do not use screws for displaced femoral neck fractures in the elderly patient. The rate of failure and reoperation rate is high for this group of patients. The type of anesthesia given to the patient is variable. It can be general or spinal anesthesia. If the fracture is displaced and unstable, then you will do hemiarthroplasty. Cemented is probably better than cementless. Cementless procedure may cause intraoperative fractures. Unipolar or bipolar procedures are controversial, however they have similar outcomes. There is no difference between bipolar and unipolar procedure except the cost (bipolar procedure is more expensive). This procedure (the prosthesis) is usually done in a patient that is physiologically old. However, total hip arthroplasty can also be done in these patients.
The pre-injury cognitive and physiologic age and function determines the optimal function after hip fracture treatment. There is a consensus that if the fracture is nondisplaced, complete or incomplete fracture, then you will treat the fracture with screw fixation. Usually at least three screws are used. The surgery is a relatively small surgery. Do not use screws for displaced femoral neck fractures in the elderly patient. The rate of failure and reoperation rate is high for this group of patients. The type of anesthesia given to the patient is variable. It can be general or spinal anesthesia. If the fracture is displaced and unstable, then you will do hemiarthroplasty. Cemented is probably better than cementless. Cementless procedure may cause intraoperative fractures. Unipolar or bipolar procedures are controversial, however they have similar outcomes. There is no difference between bipolar and unipolar procedure except the cost (bipolar procedure is more expensive). This procedure (the prosthesis) is usually done in a patient that is physiologically old. However, total hip arthroplasty can also be done in these patients.  Total hip arthroplasty is usually done in a patient with a previous hip disease or it can also be done in the older patient that is active or physiologically young. Total hip arthroplasty is usually done in a patient with a previous hip disease or it can also be done in the older patient that is active or physiologically young. Total hip will have an increased risk of dislocation. Which approach the physician will use to do the procedure is controversial. The anterolateral approach will give more fractures and abductor weakness. The posterior approach will give increased incidence of posterior dislocations and there is a need for excellent posterior capsular repair to reduce the incidence of dislocations. In general, the trend is to do cemented hemiarthroplasty.
Total hip arthroplasty is usually done in a patient with a previous hip disease or it can also be done in the older patient that is active or physiologically young. Total hip arthroplasty is usually done in a patient with a previous hip disease or it can also be done in the older patient that is active or physiologically young. Total hip will have an increased risk of dislocation. Which approach the physician will use to do the procedure is controversial. The anterolateral approach will give more fractures and abductor weakness. The posterior approach will give increased incidence of posterior dislocations and there is a need for excellent posterior capsular repair to reduce the incidence of dislocations. In general, the trend is to do cemented hemiarthroplasty. The connection between the synovial cyst and the facet joint becomes obvious. The synovial cyst is walled off from the spinal canal. The synovial cyst causes pressure on the nerve root as it tries to exit the foramen. Compare both sides. The synovial cyst acts like a herniated disc. The patient will have low back pain, numbness, and radiation of the pain down the leg. The synovial cyst is best diagnosed by an MRI. The MRI can also diagnose the compression on the nerve root by the cyst. The synovial cyst is bright in T2 MRI because it is a fluid filled mass (it’s not like an intervertebral disc) and the cyst is contiguous with the hypertrophied facet joint, which also has a high signal intensity.
The connection between the synovial cyst and the facet joint becomes obvious. The synovial cyst is walled off from the spinal canal. The synovial cyst causes pressure on the nerve root as it tries to exit the foramen. Compare both sides. The synovial cyst acts like a herniated disc. The patient will have low back pain, numbness, and radiation of the pain down the leg. The synovial cyst is best diagnosed by an MRI. The MRI can also diagnose the compression on the nerve root by the cyst. The synovial cyst is bright in T2 MRI because it is a fluid filled mass (it’s not like an intervertebral disc) and the cyst is contiguous with the hypertrophied facet joint, which also has a high signal intensity.  The synovial cyst indicates a facet pathology. The patient will be initially treated conservatively. There is a high recurrence rate with nonsurgical treatment, and if there is no improvement, then you will need to do surgery. If the patient has radiculopathy alone, do decompression. If the patient has significant low back pain due to spinal instability, you will do decompression and fusion. To check for instability, look at the MRI or the x-rays. Get flexion/extension x-rays before you decide on surgical intervention. Basically, because you have the synovial cyst and when you go in and remove the cyst, you have hypertrophy of the facets and the ligamentum flavum, so you will do a hemilaminotomy and partial facetectomy with direct decompression of the neural elements. Do fusion if there is instability.
The synovial cyst indicates a facet pathology. The patient will be initially treated conservatively. There is a high recurrence rate with nonsurgical treatment, and if there is no improvement, then you will need to do surgery. If the patient has radiculopathy alone, do decompression. If the patient has significant low back pain due to spinal instability, you will do decompression and fusion. To check for instability, look at the MRI or the x-rays. Get flexion/extension x-rays before you decide on surgical intervention. Basically, because you have the synovial cyst and when you go in and remove the cyst, you have hypertrophy of the facets and the ligamentum flavum, so you will do a hemilaminotomy and partial facetectomy with direct decompression of the neural elements. Do fusion if there is instability. This lecture is about musculoskeletal infections. A specific infection could have a specific infecting agent, a specific presentation, or a specific treatment. I am going to try to present the most common types of infections that probably has a specific thing about it. The majority of orthopedic surgical site infections (SSI) are caused by Staph Aureus.
This lecture is about musculoskeletal infections. A specific infection could have a specific infecting agent, a specific presentation, or a specific treatment. I am going to try to present the most common types of infections that probably has a specific thing about it. The majority of orthopedic surgical site infections (SSI) are caused by Staph Aureus. Chronic Paronychia. This is a fungal infection (Candida albicans). It involves an infection of the nail fold. It is common in diabetics. It does not respond to antibiotics. It occurs in people who work with water such as bartenders or dishwashers. There is really no abscess, but the area around the nail is red, tender, and swollen. It can affect multiple fingers. It should be treated with topical antifungals such as miconazole. In severe resistant cases, marsupialization should be done.
Chronic Paronychia. This is a fungal infection (Candida albicans). It involves an infection of the nail fold. It is common in diabetics. It does not respond to antibiotics. It occurs in people who work with water such as bartenders or dishwashers. There is really no abscess, but the area around the nail is red, tender, and swollen. It can affect multiple fingers. It should be treated with topical antifungals such as miconazole. In severe resistant cases, marsupialization should be done. Herpetic Whitlow occurs from the herpes simplex virus. It is a self-limited disease. It is seen in dentists, respiratory therapists, or anesthesiologists, and it can also affect toddlers. It affects some vesicles on the finger, and it will have inflammation or redness at the base of the vesicle. There is clear fluid in the vesicle, and the gram stain will be negative. You should use the Tzanck test, and the treatment is Aciclovir. Surgery is not needed.
Herpetic Whitlow occurs from the herpes simplex virus. It is a self-limited disease. It is seen in dentists, respiratory therapists, or anesthesiologists, and it can also affect toddlers. It affects some vesicles on the finger, and it will have inflammation or redness at the base of the vesicle. There is clear fluid in the vesicle, and the gram stain will be negative. You should use the Tzanck test, and the treatment is Aciclovir. Surgery is not needed. Pseudomonas Aeruginosa is commonly associated with foot punctures in children and IV drug abusers. Pseudomonas Aeruginosa infection is responsible for the majority of the osteomyelitis following nail puncture through shoes. Pseudomonas is the most characteristic cause of this infection. Treatment is incision and drainage (I&D). You must remove the foreign bodies inside and give the patient antibiotics.
Pseudomonas Aeruginosa is commonly associated with foot punctures in children and IV drug abusers. Pseudomonas Aeruginosa infection is responsible for the majority of the osteomyelitis following nail puncture through shoes. Pseudomonas is the most characteristic cause of this infection. Treatment is incision and drainage (I&D). You must remove the foreign bodies inside and give the patient antibiotics.
 Underneath the fascia can be a really terrible infection which can involve all the tissues, including the muscles, without even having a smoking gun mark on the skin surface. The blisters and the bullae are late. If you are in doubt about the presence of cellulitis or necrotizing fasciitis, do a biopsy by doing an incision down to the fascia and see if the fascia is involved (if the fascia is involved, then you have a problem). If the fascia and the muscles are involved, then you have necrotizing fasciitis. Hepatitis C is an associated risk factor for necrotizing fasciitis, and the prognosis of these patients are worse. Treatment for necrotizing fasciitis is emergency aggressive debridement. The mortality rate is high, up to 25%, and it depends on early diagnosis (mortality improves by early diagnosis and treatment). Necrotizing fasciitis is then treated with antibiotics.
Underneath the fascia can be a really terrible infection which can involve all the tissues, including the muscles, without even having a smoking gun mark on the skin surface. The blisters and the bullae are late. If you are in doubt about the presence of cellulitis or necrotizing fasciitis, do a biopsy by doing an incision down to the fascia and see if the fascia is involved (if the fascia is involved, then you have a problem). If the fascia and the muscles are involved, then you have necrotizing fasciitis. Hepatitis C is an associated risk factor for necrotizing fasciitis, and the prognosis of these patients are worse. Treatment for necrotizing fasciitis is emergency aggressive debridement. The mortality rate is high, up to 25%, and it depends on early diagnosis (mortality improves by early diagnosis and treatment). Necrotizing fasciitis is then treated with antibiotics. Gas Gangrene occurs due to Clostridium perfringens (C. perfringens). It is an anaerobic gram-positive bacilli. It is almost like every bad infection is due to gram-positive bacteria. There will be linear streaks of gas in the tissues. Gas gangrene is treated by wide debridement and leaving the wound open. It is then treated with antibiotics. Penicillin G and clindamycin are usually given.
Gas Gangrene occurs due to Clostridium perfringens (C. perfringens). It is an anaerobic gram-positive bacilli. It is almost like every bad infection is due to gram-positive bacteria. There will be linear streaks of gas in the tissues. Gas gangrene is treated by wide debridement and leaving the wound open. It is then treated with antibiotics. Penicillin G and clindamycin are usually given. Cat bites are deeper and sharper, causing deep injuries. 50% of cat bites will need surgery. Dog bites are associated with an average of five organisms (such as Pateurella Multocida and Pasteurella Canis). Dog bites cause a lot of tissue damage. Dog bites occur with incredible force, like being hit by a truck. Tearing of the tissues is visible and obvious. If the dog bite does not need debridement, you can treat it by antibiotics alone (augmentin or sophixin). The most common bacteria isolated from both dog and cat bites is pasturella multocida. The treatment is Augmentin.
Cat bites are deeper and sharper, causing deep injuries. 50% of cat bites will need surgery. Dog bites are associated with an average of five organisms (such as Pateurella Multocida and Pasteurella Canis). Dog bites cause a lot of tissue damage. Dog bites occur with incredible force, like being hit by a truck. Tearing of the tissues is visible and obvious. If the dog bite does not need debridement, you can treat it by antibiotics alone (augmentin or sophixin). The most common bacteria isolated from both dog and cat bites is pasturella multocida. The treatment is Augmentin. Some of the bacteria are grown in a special culture. Kingella kingae will grow in a blood culture. The mycobacterium avium will grow in a middlebrook medium. The E. coli will grow in a Luria-Bertani medium. Neisseria Gonorrhoeae will grow in a Chocolate Agar medium if you get it from a sterile source like joint fluid. If the specimen comes from a contaminated source, such as the vaginal swab or the urethral swab, then the medium will be Thayer-Martin Agar medium.
Some of the bacteria are grown in a special culture. Kingella kingae will grow in a blood culture. The mycobacterium avium will grow in a middlebrook medium. The E. coli will grow in a Luria-Bertani medium. Neisseria Gonorrhoeae will grow in a Chocolate Agar medium if you get it from a sterile source like joint fluid. If the specimen comes from a contaminated source, such as the vaginal swab or the urethral swab, then the medium will be Thayer-Martin Agar medium. Lymes Disease is caused by Spirochete Borrelia Burgdorferi. It lives on white-tailed deer. The vector is a tick. Early on, you will get the “bullseye” (erythema migrans). In orthopedics, we get the chronic inflammatory arthritis, the knee will be swollen but not too painful. You can get Bell’s palsy. It can be treated with antibiotics. If the patient is less than eight years old, give them amoxicillin. If the patient is older than eight years old, give doxycycline (in little kids, doxycycline will create staining of the teeth). The period to give antibiotics is between 3-6 weeks.
Lymes Disease is caused by Spirochete Borrelia Burgdorferi. It lives on white-tailed deer. The vector is a tick. Early on, you will get the “bullseye” (erythema migrans). In orthopedics, we get the chronic inflammatory arthritis, the knee will be swollen but not too painful. You can get Bell’s palsy. It can be treated with antibiotics. If the patient is less than eight years old, give them amoxicillin. If the patient is older than eight years old, give doxycycline (in little kids, doxycycline will create staining of the teeth). The period to give antibiotics is between 3-6 weeks. Sporotrichosis, or rose gardener’s disease, is caused by a fungus called sporothrix. It occurs in people who grow roses. The injury occurs from thorns or splinters. You can get granulomas, nodules, ulcers, or lymphatic spread. H&E staining will show an asteroid body. It can be treated by debridement, amphotericin B, or potassium iodide.
Sporotrichosis, or rose gardener’s disease, is caused by a fungus called sporothrix. It occurs in people who grow roses. The injury occurs from thorns or splinters. You can get granulomas, nodules, ulcers, or lymphatic spread. H&E staining will show an asteroid body. It can be treated by debridement, amphotericin B, or potassium iodide.