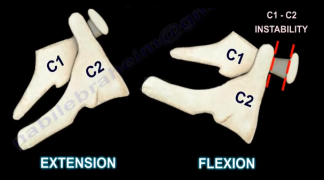
A physeal injury in the distal femur in the neonate is rare. In general, traumatic neonatal physeal fracture usually occurs in the distal humerus and rarely occurs in the distal femur. The condition usually occurs due to birth trauma and usually results due to physeal separation which results in epiphyseal separation. The thigh will be swollen and there may be hypomobility of the extremity. The neonate will be fussy or irritated with significant swelling in the thigh. The condition is under diagnosed. The epiphysis is usually present at birth on x-rays. This condition can become complicated if the epiphysis is not completely ossified at birth or if the child is born prematurely. In this situation, the x-ray interpretation may be difficult. An MRI will be really helpful if the doctor is uncertain of the diagnosis. X-rays should be taken at the child at birth. The physician should look at the lateral x-ray and find the epiphysis is present and ossified at birth with varying degrees (may not be clear). Each epiphysis will line up with its corresponding bone. Epiphysis of the distal femur should line up with the femoral  shaft. Epiphysis of the proximal tibia should line up with the tibial shaft. If the two epiphysis separate from each other, then this is a congenital dislocation of the knee. This can be a spectrum of injury that varies from hyperextension to subluxation, to frank dislocation. If the epiphysis is separated from its corresponding bone, for example, the epiphysis of the distal femur is separated from the shaft of the femur, then this is a physeal injury. Because the distal femur is mostly cartilaginous, you don’t see bone shifting, you see a little hint of the separation of the physis by seeing that the small ossified epiphysis is not in its normal position that corresponds with the axis of the bone. You need to know the difference between physeal injury and congenital dislocation of the knee. Accurate, gentle closed reduction with follow-up x-rays to confirm the reduction and to detect any early bony bridging.
shaft. Epiphysis of the proximal tibia should line up with the tibial shaft. If the two epiphysis separate from each other, then this is a congenital dislocation of the knee. This can be a spectrum of injury that varies from hyperextension to subluxation, to frank dislocation. If the epiphysis is separated from its corresponding bone, for example, the epiphysis of the distal femur is separated from the shaft of the femur, then this is a physeal injury. Because the distal femur is mostly cartilaginous, you don’t see bone shifting, you see a little hint of the separation of the physis by seeing that the small ossified epiphysis is not in its normal position that corresponds with the axis of the bone. You need to know the difference between physeal injury and congenital dislocation of the knee. Accurate, gentle closed reduction with follow-up x-rays to confirm the reduction and to detect any early bony bridging.